Hypertension is the leading cause of cardiovascular disease. About 9.4 million deaths worldwide are due to hypertension1. In Singapore, about one in four persons have been diagnosed with hypertension, and there is a higher prevalence in persons above 40 years of age2.
By Dr Mohammed Rizwan Amanullah, Consultant, Department of Cardiology
Our circulatory system comprises the heart as the central pumping organ which pumps blood into the arteries. This blood column moves forward in arterial system and reaches capillaries at tissue level where nutrient and oxygen exchange occur and finally returns to the heart via the venous system. Blood pressure (BP) refers to pressure exerted by the column of blood on the vessel walls. Clinically, it is the arterial BP which is important, and this is recorded by either direct or indirect measurements.
Recording of Blood Pressure
i) Direct measurements: Invasive monitoring devices using an intra-arterial monitoring line connected to a transducer. This is performed in intensive care units where a constant
monitoring of BP is needed.
ii) Indirect measurements: Using different types of sphygmomanometers.These include the mercury sphygmomanometers, automated BP devices and ambulatory BP recording devices.
When BP is elevated beyond the acceptable physiological limits, then a diagnosis of high BP or hypertension is made. However, elevated BP readings must be confirmed on at least a minimum of two separate occasions and at least 1 to 4 weeks apart. BP is measured in units of millimeters of mercury (mmHg) and the readings are always in pairs, with the upper (systolic) value and the lower (diastolic) value.
Guide to Measuring BP
BP monitoring devices are readily available and do not need a prescription. It is important to know the proper steps to taking BP to ensure an accurate measurement of BP and manage high BP.
General Principles to Measuring BP:
i) Stay well rested for at least 5 to 10 minutes prior to taking BP. If you had just exercised, you are recommended to rest for at least 30 minutes.
ii) Preferably no smoking, consumption of heavy meals or caffeinated drinks within 30 minutes preceding the measurement.
iii) Empty your bladder before taking BP.
iv) Take the measurement in a sitting position, with arm rested by the side on a table, and feet on the floor with legs uncrossed.
v) The BP cuff should be tied against the bare skin, and it should fit tightly.
vi) Arm should be rested at the same level as the heart (figure 1).
Measure your BP at least 2 to 3 times at one-minute intervals for accurate readings.
An inaccurate measurement of BP may occur in the following situations:
i) When you are feeling anxious
ii) BP taken immediately after a meal or caffeine intake
iii) Improper body position
iv) Inappropriate cuff size
v) Faulty BP monitoring device
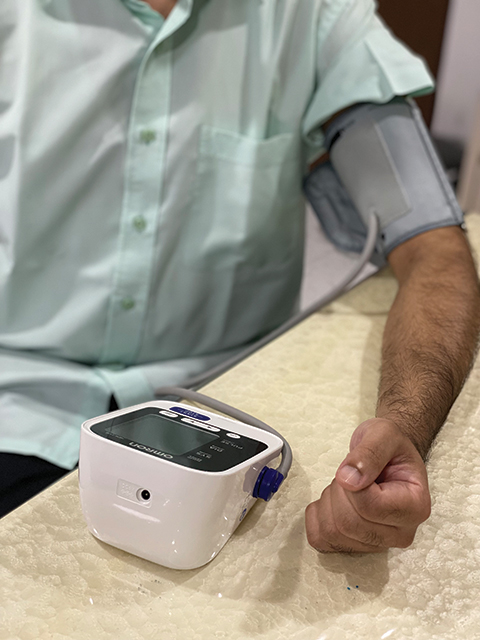
Figure 1: Correct positioning of measuring BP
Choosing the Right BP Cuff:
There are different sizes of BP cuffs. Most of the readily available home BP monitors come with standard adult-sized cuffs. A rough guide used is that the length of ladder of the cuff should encircle at least 80% of circumference of upper arm, and its width should be at least 40% of upper arm circumference (table 1).
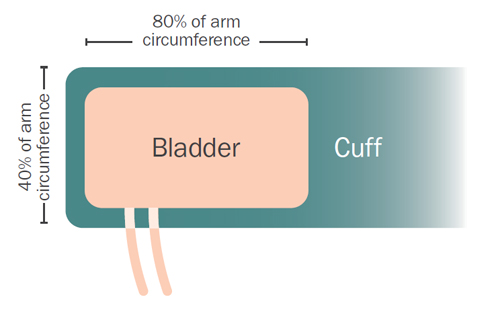
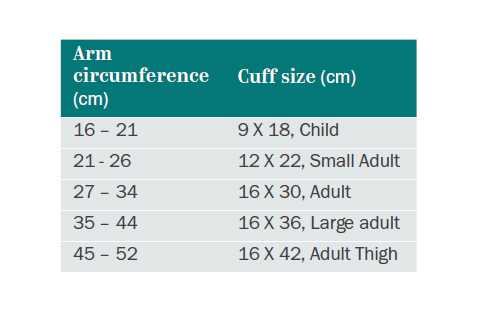
Table 1: Recommended BP cuff sizes based on arm circumference 3, 5
A medium-sized cuff should suffice for most adults. A large-sized cuff should be considered for those who are obese. Improper cuff size will lead to erroneous measurements of BP.
Monitoring BP with Acceptable BP Variations
BP readings are recommended to be measured and recorded at the same timing daily, for those who are advised to monitor their BP. BP is lowest on waking up in the morning and tends to increase with physical activity during daytime. During sleep, there is a physiological reduction in BP by 10 – 15% of the daytime readings and this is referred as nocturnal dipping.
Hypertension: Primary and Secondary
Hypertension rarely causes symptoms and hence it is often picked up incidentally upon screening. Occasionally, some persons may manifest late with uncontrolled hypertension and have symptoms of breathlessness, headaches, blurring of vision and nose bleeding.
There are mainly two types of hypertension – primary and secondary hypertension. Primary (essential) hypertension is the most common type and has no underlying cause. Secondary hypertension, on the other hand, is caused by underlying conditions or use of certain medications.
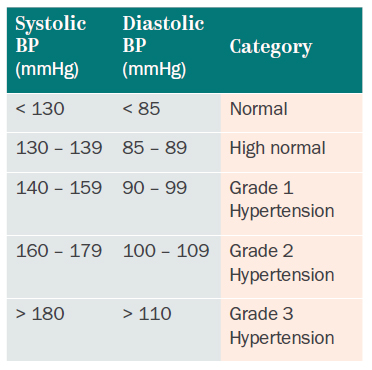
The cut-off readings for the hypertension diagnosis have become more stringent in the recent years (as depicted in table 2) because early diagnosis and treatment of hypertension helps to reduce the complications. If only systolic or diastolic reading is elevated, BP is graded based on the higher reading among the two. Note that the cut-off readings for ambulatory BP are slightly different for diagnosis of hypertension.
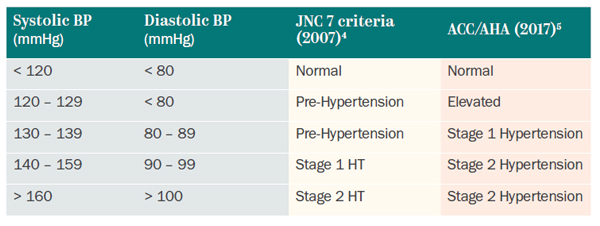
Table 2: International criteria for diagnosis of hypertension.
Locally, the definition of hypertension as per Ministry of Health6 depicted as below:
Evaluating and Treating Hypertension
A detailed history and physical examination are necessary to assess for any symptoms or complications of organ damage. Additional tests such as electrocardiogram (ECG), urine tests, kidney function tests would also be required to screen for other concomitant risk factors like diabetes mellitus, high cholesterol (hyperlipidemia). Depending on the suspected secondary causes, more detailed investigations are needed.
It is important to treat hypertension. Untreated hypertension can lead to organ damage and cause complications like stroke, heart attack, retinopathy (affecting eye vessels and vision), lower limb peripheral arterial disease, and kidney damage. Managing and keeping good control of BP can reduce the incidence of coronary artery disease and stroke in the long term. The physician will assess and recommend the appropriate medication options based on age, other associated risk factors, and any pre-existing end organ damage. Besides medications, diet and lifestyle modifications are important in managing the condition.
1 Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013; 380:2224-2260.
2 Epidemiology and Disease Control Division Ministry of Health Singapore. National Health Survey 2010 Report.
3 M. Halm. Arm circumference, shape, and length: how interplaying variables affect blood pressure measurement in obese persons. American journal of critical care. 2014.
4 The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). US dept of Health and Human services, NIH: December 2003 in Hypertension. 2003;42:1206
5 Paul K. Whelton, Robert M. Carey, Wilbert S. Aronow, Donald E. CaseyJr, Karen J. Collins, Cheryl Dennison Himmelfarb, Sondra M. DePalma, Samuel Gidding, Kenneth A. Jamerson, Daniel W. Jones, Eric J. MacLaughlin, Paul Muntner, Bruce Ovbiagele, Sidney C. SmithJr, Crystal C. Spencer, Randall S. Stafford, Sandra J. Taler, Randal J. Thomas, Kim A. Williams Sr et al. ACC/AHA/AAPA/ABC/ACPM/AGS/AphA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115
6 MOH clinical practice guidelines on Hypertension - November 2017
This article is from Murmurs Issue 40 (May – August 2021). Click here to read the full issue.
